The Centers for Medicare & Medicaid Services (CMS) is taking a harder line on how states use Medicaid dollars, especially when it comes to caring for undocumented individuals. While the move is framed as a matter of fiscal accountability, it lands squarely in the middle of an already fragile healthcare ecosystem.
Federal law has long limited Medicaid coverage for undocumented immigrants to emergency care only. However, CMS says some states have gone further than the law allows, expanding benefits and passing the cost onto federal taxpayers. CMS says that has to stop.
“Medicaid is not, and cannot be, a backdoor pathway to subsidize open borders,” said CMS Administrator Mehmet Oz, MD, on May 27. “States have a duty to uphold the law and protect taxpayer funds.”
What’s Changing—and Why It Matters
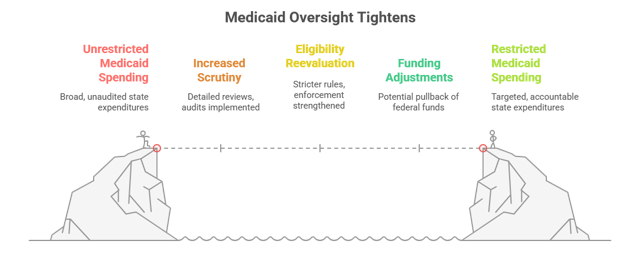
To enforce these boundaries, CMS is rolling out a series of oversight actions:
- More detailed reviews of state Medicaid spending (CMS-64 reports)
- Audits of state financial systems
- Reevaluations of eligibility rules to close gaps and strengthen enforcement
States are being told to tighten their systems, modernize how they manage eligibility, and ensure every Medicaid dollar is being spent as intended. If they don’t, they risk CMS stepping in and pulling back federal funding.
But this isn’t just about numbers on a spreadsheet—it’s about people.
The Real-World Impact: A Chilling Effect on Care
Hospitals and healthcare systems are raising red flags. As oversight ramps up and rhetoric around immigration intensifies, there’s growing concern that eligible patients, especially those in mixed-status families, will be too afraid or confused to seek the help they need. Even lawful residents or U.S. citizens may hesitate to apply for benefits if they fear unintended consequences for themselves or their loved ones.
And when people delay care or skip coverage entirely, they often end up in the emergency room. That’s where hospitals step in, whether they’re paid or not.
This could be devastating for hospitals that already serve high volumes of Medicaid and uninsured patients. These facilities operate on the thinnest of margins and rely heavily on Disproportionate Share Hospital (DSH) payments to stay afloat. If Medicaid enrollment drops and federal oversight intensifies, it could lead to:
- More uninsured patients
- Less federal funding flowing to states and hospitals
- Rising uncompensated care that exceeds DSH reimbursement limits
- A real financial crisis for hospitals that care for the most vulnerable
So What Now?
This moment requires more than compliance from healthcare leaders; it demands clarity and strategy.
Hospitals must take stock of their exposure, shore up outreach efforts to help eligible patients enroll confidently, and advocate at the state level for policies that protect critical funding streams like DSH.
Just as importantly, it’s time to lean on trusted partners, those who understand the regulations and the human realities behind them. Navigating eligibility, protecting funding, and building outreach strategies that are both effective and empathetic isn’t easy, but it’s necessary.
The Bottom Line
The mission hasn’t changed: care for those who need it most.
This moment is bigger than policy. It’s about ensuring that fear doesn’t override access. It’s about ensuring hospitals can keep their doors open and doing what they were built to do.
In the end, it’s not just about Medicaid dollars. It’s about the people behind them.

Leave A Comment
You must be logged in to post a comment.