The Centers for Medicare & Medicaid Services (CMS) has launched a nationwide initiative aimed at strengthening eligibility oversight for Medicaid and the Children’s Health Insurance Program (CHIP). This effort focuses on ensuring that only eligible individuals remain enrolled.
At Resource Corporation of America (RCA), we recognize the new challenges this poses to hospitals and health systems.
What’s Changing
Enhanced Verification
CMS will now provide states with monthly enrollment reports highlighting individuals whose citizenship or immigration status cannot be confirmed through federal databases, including the Department of Homeland Security’s SAVE (Systematic Alien Verification for Entitlements) system.
States must then:
- Review flagged enrollment cases.
- Request additional documentation as needed.
- Take corrective action, such as adjusting coverage or applying non-citizen eligibility rules.
CMS will closely monitor progress, requiring states to show timely compliance with federal eligibility standards.
Limited Services for the Ineligible
Individuals who do not meet the citizenship or immigration status requirements will only qualify for emergency-related limited services. This reaffirms CMS’ commitment to ensuring consistency in federal eligibility enforcement across all states.
Implications for Hospitals & Health Systems
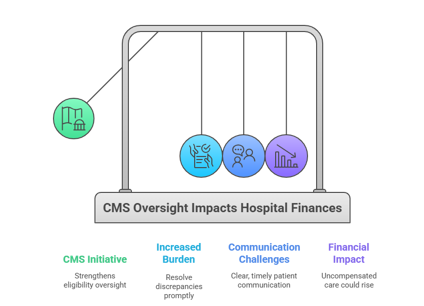
For hospitals, this initiative carries several practical implications:
- Increased Administrative Burden: Hospitals and state agencies must resolve discrepancies promptly, accurately document verification activities, and maintain compliance.
- Patient Communication Challenges: Patients flagged in monthly reviews will require clear and timely communication to prevent confusion or gaps in care.
- Financial Impact: As coverage lapses for ineligible patients, uncompensated care could rise—putting additional strain on hospital resources.
RCA’s Perspective
At RCA, we see this as both a challenge and an opportunity for our hospital partners. While states and facilities must increase oversight efforts, RCA is uniquely positioned to help navigate these changes. We have seen this before, and as an industry, we must adapt to these new requirements.
- We specialize in assisting self-pay and uninsured populations in qualifying for Medicaid, CHIP, and other assistance programs.
- Our teams are adept at managing complex documentation requirements and resolving eligibility discrepancies.
- By partnering with companies like RCA, hospitals can mitigate risks of uncompensated care while ensuring compliance with the heightened federal scrutiny.
Looking Ahead
This initiative makes it clear: eligibility compliance will remain a central focus of federal oversight for Medicaid and CHIP. For hospitals and health systems, partnering with an experienced eligibility vendor is now more critical than ever.
We view these regulatory shifts as part of doing business. Over our 30-year history, we’ve seen the pendulum swing many times, and we are fully prepared to adapt and deliver under today’s rules. RCA’s mission remains unchanged…helping patients secure the coverage they qualify for while protecting hospital financial stability.

Leave A Comment
You must be logged in to post a comment.