For over a million Americans living with disabilities, accessing Social Security Disability Insurance (SSDI) or maintaining Medicaid coverage isn’t just difficult; it’s starting to feel impossible.
In recent months, the Social Security Administration (SSA) has found itself in a perfect storm: historic backlogs, alarming staff reductions, and widespread office closures. The average wait time for an initial disability claim decision now exceeds 230 days. The process can stretch well beyond two years if a hearing is needed.
Let that sink in: two years to determine whether you qualify for basic benefits.
In 2023 alone, 30,000 people died while waiting for Social Security disability benefits.
And in 2025, things took another turn. SSA announced the elimination of 7,000 positions, over 12% of its workforce, alongside the closure of 60% of its regional offices and even the Office of Civil Rights and Equal Opportunity shutdown. Phone services are vanishing, pushing people to online portals or in-person visits that may require traveling over 100 miles. For someone living with a disability, that’s not just inconvenient; it can be prohibitive.
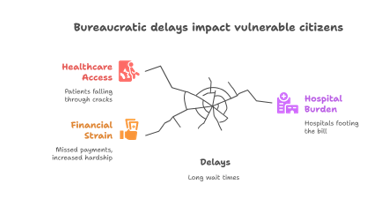
This isn’t a change in benefit levels. But when access becomes this strained, the outcome feels the same: missed payments, increased hardship, and patients falling through the cracks.
Medicaid Misconceptions—and the Real Threat
Meanwhile, Medicaid expansion continues to draw fire, but the data tells a different story. Despite concerns that expanding Medicaid might strain disability services or lengthen waitlists, the opposite appears true. States with Medicaid expansion are more likely to avoid home and community-based services (HCBS) waitlists, while the most considerable delays exist in non-expansion states like Texas and Florida.
The more pressing threat isn’t expansion; it’s cuts. Ongoing federal budget talks propose deep reductions in Medicaid funding, which could destabilize support systems for some of the most vulnerable.
Another hidden trap? Many Medicaid Buy-In programs penalize people with disabilities for working too much or saving too much. These income and asset caps create a “poverty trap,” forcing individuals to choose between pursuing a career and keeping their healthcare. Fortunately, states like Iowa are now considering laws modeled after Tennessee to loosen these restrictions and support economic independence.
Why This Matters for Hospitals…and How RCA Helps
These policy changes and operational shortfalls have a tangible impact on hospitals and health systems. When patients are delayed in accessing Social Security benefits or Medicaid coverage, hospitals often end up footing the bill.
That’s where organizations like Resource Corporation of America step in.
At RCA, we help hospitals identify and qualify patients eligible for Medicaid, SSDI, or hospital-based charity programs. Our team monitors these policy shifts closely because hospitals need someone to navigate the fine print when the rules change. Whether helping a self-pay patient find retroactive Medicaid coverage or working with a disability applicant facing long SSA delays, our focus is the same: maximize recoveries, reduce write-offs, and support patient access to care.
In a complex and increasingly unstable system, having a partner who understands the landscape isn’t optional. It’s essential.
Want to Learn More?
Let’s talk if your hospital sees more patients stuck in limbo, uninsured, underinsured, or waiting on decisions from overburdened government systems. RCA has been helping hospitals and their patients navigate Medicaid and disability benefits for over 30 years. Let us help you bridge the gap.

Leave A Comment
You must be logged in to post a comment.