If you rely on Medicaid Disproportionate Share Hospital (DSH) funding, the next 12 months will matter. The American Hospital Association’s latest fact sheet flags significant reductions to Medicaid DSH starting Oct. 1, 2025 (FY 2026), with additional cuts slated for FY 2027–2028. Pair those reductions with persistent Medicaid underpayment and new limits on certain supplemental payments under the OBBBA, and you get a tighter operating environment for safety-net care.
The short version
- $8B DSH cut hits FY 2026 (effective Oct. 1, 2025); another $8B in FY 2027 and $8B in FY 2028.
- Hospitals already faced a $27.5 billion Medicaid shortfall in 2023, representing the gap between Medicaid payments and the actual cost of care.
- OBBBA-driven limits on state-directed payments will further constrain non-DSH supplemental dollars that many systems use to plug holes.
- Net: more exposure to uncompensated care and cash-flow volatility unless eligibility capture, enrollment, and charity/coverage pathways are maximized.
What changed and why it matters
The DSH program exists to offset the costs of caring for uninsured and under-insured patients, including those covered by Medicaid. DSH was trimmed in the ACA era under the assumption that coverage expansion would suppress uncompensated care. That assumption hasn’t been fully realized, and coverage churn remains a live issue. With OBBBA provisions prompting state program changes and limiting certain supplemental payment tools, DSH is becoming even more important just as it’s being cut.
For RCA client facilities, this translates into:
- Budget pressure as DSH dollars decline while payer mix remains challenging.
- Higher stakes for front-end enrollment.
- Greater need for disciplined presumptive charity pathways to avoid avoidable bad debt.
- Cash-flow timing risk if back-end denials rise or enrollment steps stall.
What we’re doing for you
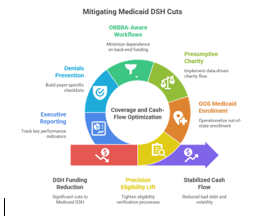
We’re approaching this as a coverage and cash-flow problem with a systemwide, measurable response:
- Precision Eligibility Lift (Primary & Secondary)
Tighten eligibility verification at order, scheduling, and pre-service checkpoints. We aim to raise Medicaid hit rates and identify secondary coverage (COB) that’s often missed, especially in multi-plan markets and for managed care carve-outs. - Out-of-State Medicaid Enrollment & Billing
Patients cross borders, and so should your reimbursement. We operationalize OOS enrollment, portal navigation, and required documentation so you can bill the right program the first time and reduce aged AR. - Presumptive Charity & Financial Counseling at Scale
Where coverage doesn’t exist, we operationalize a two-lane charity flow: presumptive (data-driven) and documentation-required (counseled). This preserves community goodwill, improves compliance, and prevents inappropriate bad debt conversions. (Flat-fee or hybrid models available.) - OBBBA-Aware Workflows
Because non-DSH supplemental options are tightening, we front-load coverage resolution to minimize dependence on constrained back-end funding streams. We align facility SOPs to the new realities so fewer accounts are left hoping for supplemental fixes later. - Denials Prevention, Not Just Appeals
Denials that cite eligibility, enrollment, plan mismatch, or COB are largely preventable. RCA builds payer-specific checklists into pre-bill QC and uses exception queues for high-risk accounts so corrections happen before first submission. - Executive-Ready Reporting
Weekly dashboards track hit rate, secondary coverage finds, OOS approvals, charity determinations, and first-pass yield, plus an ROI roll-up that shows how these actions offset projected DSH exposure.
What good looks like
- Eligibility hit rate: sustained lift of 2–5+ percentage points (market-dependent).
- Secondary coverage detection: double-digit increase in COB identifications within 60–90 days.
- First-pass yield: measurable reduction in eligibility/enrollment-related denials within two cycles.
- Bad debt containment: higher charity conversion where appropriate, with documented financial assistance compliance.
Immediate steps for client facilities
- Baseline the gap: quantify your FY 2026–2028 DSH exposure versus recent supplemental flows.
- Map the front door: identify where eligibility is checked (and where it isn’t)—orders, scheduling, pre-reg, POS, and post-discharge.
- Sort the OOS backlog: flag every account with a plausible out-of-state Medicaid pathway; we’ll fast-track the highest-yield programs first.
- Tune presumptive charity: confirm your data sources, scoring thresholds, and appeal logic; ensure compliance alignment.
- Stand up a 90-day sprint: pick 2–3 service lines and a subset of payers for rapid cycle improvement with clear KPIs.
Our commitment
RCA exists to protect coverage, stabilize cash flow, and reduce avoidable bad debt. As DSH dollars tighten, the facilities that win will be the ones that treat eligibility, enrollment, and charity as a unified operating system, not a set of disconnected tasks. We’ll bring the people, process, and tech to make that system hum, and we’ll prove impact with transparent reporting your finance team can trust.
“RCA is the single best solution for Third Party Eligibility Services.”

Leave A Comment
You must be logged in to post a comment.