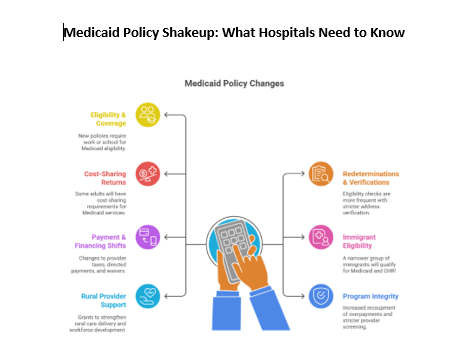
A lot is happening in the Medicaid policy world, and as your trusted partner in revenue cycle optimization, we’re keeping close watch on what’s coming. Here’s a quick rundown of significant Medicaid changes and how they may impact hospitals, patients, and the communities we serve:
Tightening Eligibility & Coverage Rules
New federal policies will require expansion of adults (ages 19-64) to work 80+ hours per month or attend school part-time to qualify for Medicaid. Certain groups, parents of young kids, individuals in treatment, or medically frail patients, will be exempt. States must verify compliance regularly and can’t waive these requirements. Notably, anyone disenrolled for not meeting the criteria will also be ineligible for Marketplace subsidies.
Faster Redeterminations, Stricter Verifications
Eligibility checks will now occur every six months for expansion adults, rather than annually. States must also verify enrollees’ addresses using tools like the National Change of Address database and cross-check to prevent individuals from being enrolled in more than one state. Retroactive coverage will be reduced to just one or two months.
Cost-Sharing Returns for Some
States will be required to charge Medicaid expansion adults with incomes between 100% and 138% of the federal poverty level up to $35 per service. Primary care, mental health, and substance use services will remain exempt, as will services provided by rural or behavioral health clinics.
Restrictions on Immigrant Eligibility
Only a narrower group of lawfully present immigrants will qualify for Medicaid and CHIP. Those without green cards, or not covered under specific exceptions, could be excluded from eligibility, including some groups who previously qualified under waivers or special status.
Key Payment & Financing Shifts for States and Providers
- Provider Taxes: States can no longer create new provider taxes or increase existing ones. Safe harbor limits for expansion states will shrink gradually to 3.5%.
- Directed Payments: States will be capped at Medicare-equivalent payment levels when directing MCO payments to hospitals and nursing facilities.
- Section 1115 Waivers: CMS’ Chief Actuary must certify all new waivers don’t increase federal costs, tightening budget neutrality requirements.
Focus on Program Integrity
Expect more frequent recoupment of overpayments, stricter provider screening (including deceased provider checks), and elimination of payments to certain reproductive health providers like Planned Parenthood (pending ongoing litigation).
New Opportunities & Support for Rural Providers
Amidst cuts, there’s a silver lining. The Rural Health Transformation Program is allocating $50 billion in grants (through 2030) to strengthen rural care delivery, including support for hospitals and workforce development.
Looking Ahead
These changes are estimated to cut federal Medicaid spending by over $900 billion in the next decade. As policies evolve, RCA remains committed to helping hospitals navigate the shifting landscape, identifying coverage opportunities, managing eligibility workflows, and protecting the financial sustainability of the safety net.

Leave A Comment
You must be logged in to post a comment.