Team A: Team B: Kersten Bartelt, RN; Neil Sandberg EpicResearch.org
Key Findings:
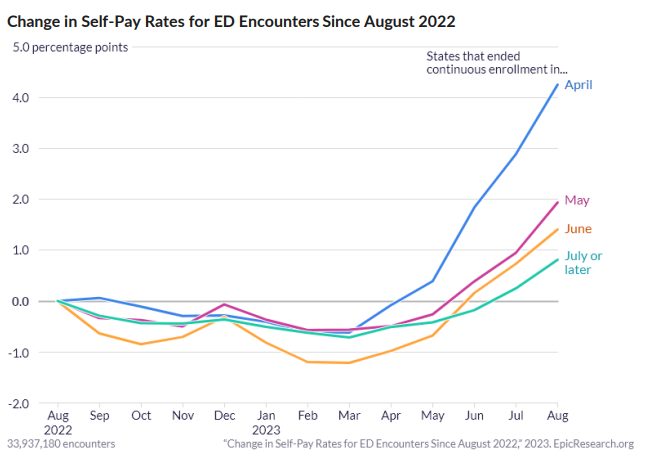
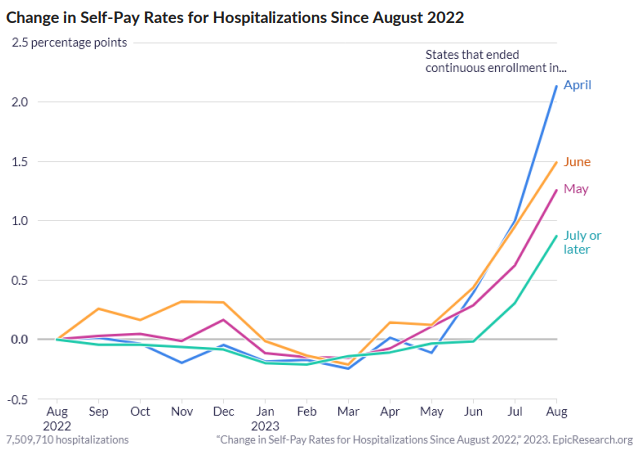
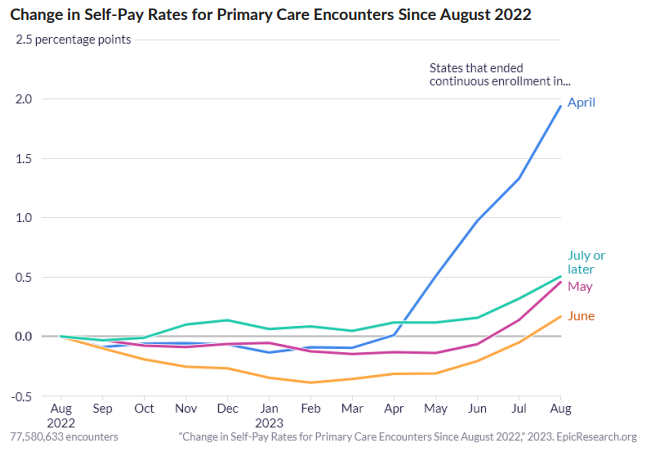
• The proportion of self-pay emergency department (ED), hospital, and primary care encounters
increased starting in April 2023 when states could start terminating Medicaid coverage for
patients who no longer met Medicaid requirements following the pandemic.
• Rates of self-pay encounters have increased the most for patients in states that began terminating
coverage in April 2023, but encounters for patients in states that started terminating coverage in
May and later appear to be following similar trends of increased rates of self-pay encounters.
During the COVID-19 pandemic period, the U.S. federal government authorized a temporary increase in
the amount of funding that states could receive for medical assistance, provided the state kept nearly all
current Medicaid patients enrolled in coverage throughout the pandemic.1 That condition expired at the
end of March 2023, when states could begin to terminate coverage for patients who no longer met
eligibility requirements for Medicaid. Several states began reviewing eligibility and started terminations of
coverage in April 2023, but states have until the end of March 2024 to resume to normal eligibility
conditions.
A study published by KFF found that, prior to the pandemic, 65% of patients whose Medicaid coverage
ended did not have insurance coverage in the following year. Lack of insurance coverage could result in
expensive medical bills for patients who are required to pay for their healthcare out of pocket.
To understand how coverage trends have changed since Medicaid terminations started again in April 2023, we analyzed 34 million hospitalizations, 340 million primary care encounters, and 146 million ED
encounters that occurred between January 2017 and August 2023 to determine the proportion of self-pay
encounters by the month Medicaid coverage terminations started in each state.
We measured how much the percentage of self-pay encounters deviated from the percentage of self-pay
encounters that occurred in August 2022 for each encounter type, as seen in Figure 1. Across all three
encounter types, states that ended continuous enrollment in April 2023 have had the greatest increase in
self-pay visits in August 2023 compared to August 2022. States that ended continuous enrollment in May
or June 2023 have had similar shifts in their self-pay trends. States that ended in July or later are starting
to show early indications of an increased proportion of self-pay encounters across all three encounter
types studied. If the current trend continues, the proportion of self-pay covered encounters will rise for all
three encounter types.
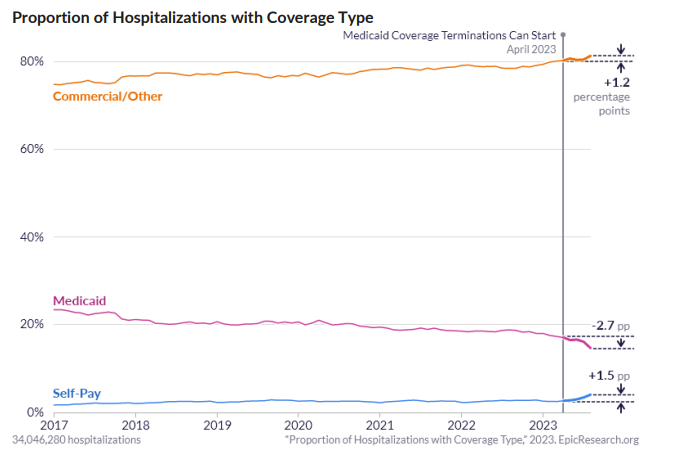
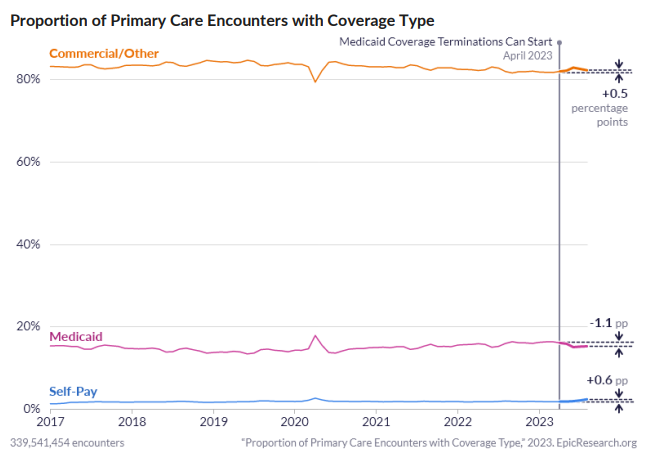
To further understand how Medicaid terminations may be influencing trends in insurance coverage, we
measured the monthly rates of encounters covered by either Medicaid or by another insurer compared to
self-pay from January 2017 to August 2023.
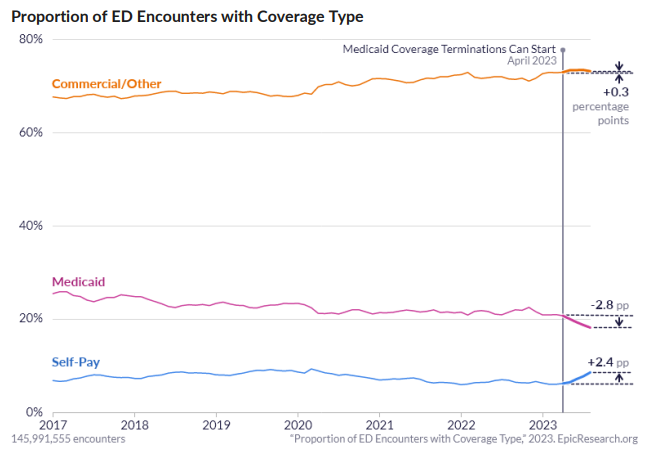
The proportion of ED encounters with Medicaid coverage decreased by 4.4 percentage points between
January 2017 and March 2023 from around 25% to 21%. The proportion of ED encounters with Medicaid
coverage decreased by 2.8 percentage points from March 2023 to August 2023. We also saw an increase
of 2.4 percentage points for self-pay and 0.3 percentage points for commercial/other ED encounters from
March 2023 to August 2023, which suggests that most of the Medicaid ED volume transitioned to selfpay.
The proportion of hospitalizations with Medicaid coverage has trended downward by 6.2 percentage
points from 23% of hospitalizations in 2017 to less than 18% in March 2023. Between March and August
of 2023, the proportion dropped an additional 2.7 percentage points. This coincided with a 1.5 percentage point rise in the proportion of self-pay hospitalizations and a 1.2 percentage point increase in
commercial/other coverage.
between 14 and 15% since 2017 with a small spike to 16% at the start of the pandemic. The proportion of
self-pay primary care encounters increased slightly over time to about 2% in 2019, where it remained until
March 2023. The proportion of self-pay encounters increased by 0.6 percentage points between March
2023 and August 2023. Commercial/other insurance-covered encounters make up the other 0.5
percentage point difference since the end of continuous enrollment for Medicaid.
These data come from Cosmos, a collaboration of 222 Epic health systems representing over 220 million patient records from 1,272 hospitals and more than 27,200 clinics from all 50 states and Lebanon. This study was completed by two teams that worked independently, each composed of a clinician and research scientists. The two teams came to similar conclusions.
Graphics by Brian Olson.
References
- Unwinding and returning to regular operations after COVID-19. (n.d.). Medicaid.gov.
https://www.medicaid.gov/resources-for-states/coronavirus-disease-2019-covid-19/unwinding-andreturning-regular-operations-after-covid-19/index.html. Accessed September 20, 2023. - https://www.kff.org/medicaid/issue-brief/how-many-people-might-lose-medicaid-when-statesunwind-continuous-enrollment/https://www.kff.org/medicaid/issue-brief/what-happens-afterpeople-lose-medicaid-coverage/Corallo, B., Burns, A., Tolbert, J., & Claxton, G. (2023, January 25).
What happens after people lose Medicaid coverage? KFF. https://www.kff.org/medicaid/issuebrief/what-happens-after-people-lose-medicaid-coverage/. Accessed October 5, 2023.https://www.kff.org/medicaid/issue-brief/what-happens-after-people-lose-medicaid-coverage/

Leave A Comment
You must be logged in to post a comment.